Visionaries transform eye research
For more than three decades, the Save Sight Institute has been world leader in eye research. Professor Peter McCluskey knows how important bequests have been to achieving its many breakthroughs.
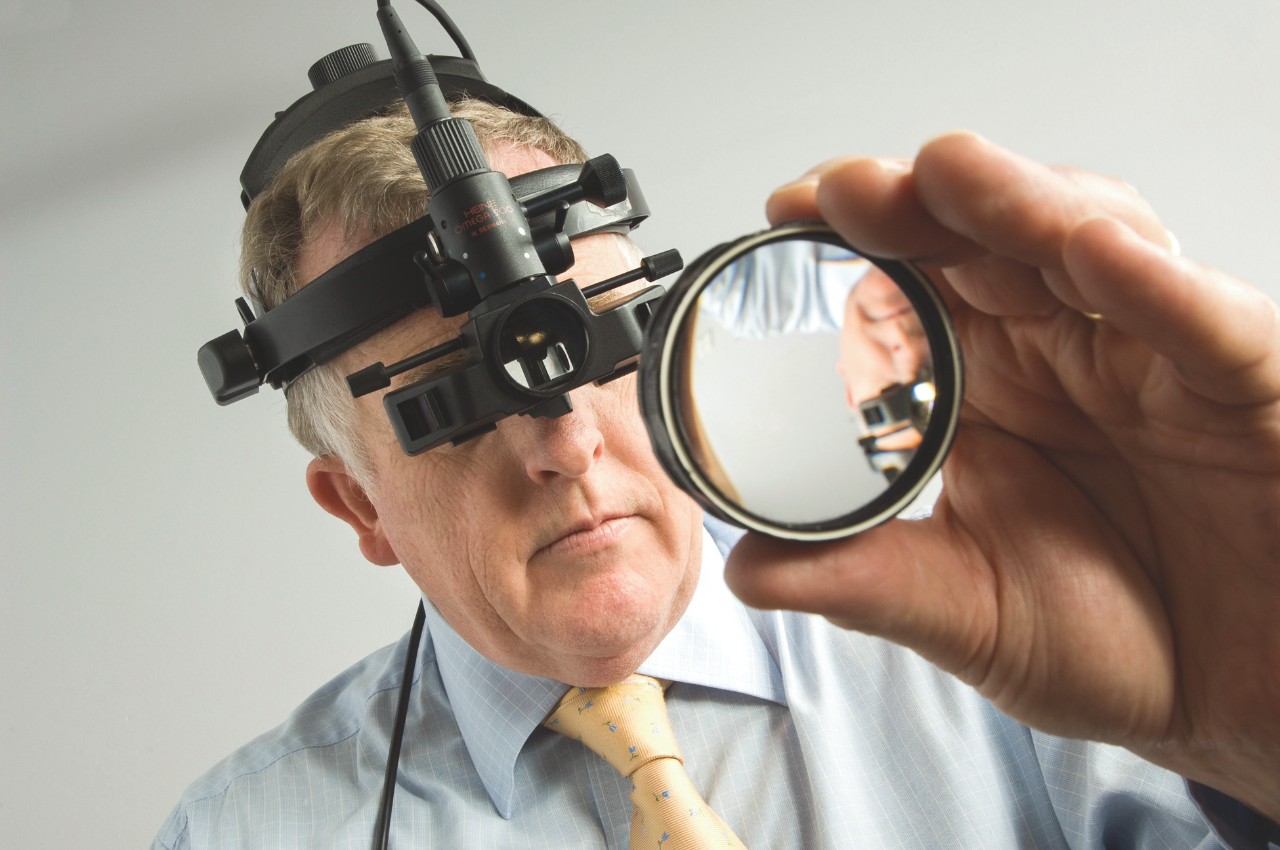
Professor Peter McCluskey.
“Having good vision is critically important – if you can see well, you will age well and age productively,” says Peter McCluskey, Professor of Clinical Ophthalmology and Eye Health, and Director of the Save Sight Institute. The institute forms part of the University of Sydney Medical School, and incorporates the University’s Discipline of Clinical Ophthalmology, which is responsible for the teaching of ophthalmology and research skills to undergraduate and postgraduate medical, ophthalmology, research and vision science students. Through the discipline of ophthalmology, the Save Sight Institute is responsible for training 80 percent of ophthalmologists in NSW.
The institute’s clinic provides specialist services across the spectrum of ophthalmic conditions, with a focus on rare eye conditions, specialist investigations and research. As a tertiary referral centre, the clinic attracts the most severe and complex eye disorders, and leads research into eye diseases and conditions throughout Australia and overseas. Its renowned team of researchers and doctors is at the forefront of ophthalmic breakthroughs, and their findings have saved the sight of many people living with eye disease since the institute was formed in 1985.
Some of this research includes the use of intravitreal steroids for macular diseases. The first clinical trials were conducted at the institute in the 1990s, and their use is now ‘standard of care’ treatment for many different macular diseases. “Intraocular steroids have been applied to diabetic retinopathy, macular oedema and retinal vascular disease. It has revolutionised the outcomes of many of those diseases,” Professor McCluskey says.
“People who have vision impairment, or who are legally blind with severe vision impairment, have much higher rates of depression, falls, hip fractures, and hospital admissions,” he adds. “If you can’t see you become socially isolated, you become reliant on others, and you lose independence.”
With a team motivated to minimise the impacts of eye disease and related conditions, Professor McCluskey says the institute relies on the generosity of its benefactors.
“Bequests and donations are critically important to our ability to flourish as a research institute,” he says. “Bequests such as Diana Mackintosh’s for macular degeneration research are vital for us, and this one came at a timely moment.”
Ms Mackintosh’s substantial donation of almost $300,000 will support the Macular Research Group, which develops new treatments to reduce the prevalence of blindness from macular disease. The group is headed by Professor Mark Gillies, and made up of three cohesive research units working closely with Sydney Eye Hospital. Donations are also funding an international project, led by Professor Gillies, looking at causes of a common macular disease known as MacTel, or macular telangiectasia. Researchers are trialling potential treatments for this previously untreatable disease.

Professor Mark Gillies.
A recent donation from John and Shirley Sarks will fund a researcher in perpetuity to perform research on age-related macular degeneration, building on the Sarks’ groundbreaking research from the 1970s and 80s.
“Not only have the Sarks made a generous contribution to eye research, they have given us their collection of specimens, which is unparalleled anywhere in the world,” says Professor McCluskey. “Now we have a researcher to apply modern techniques to this disease and we’ve got the specimens on which to do it.”
Research at the institute covers all major parts of the eye and is integrated across laboratory research, clinical trials, implementation and ongoing patient monitoring. Research areas include cataract, corneal, eye cancer, lens development, macular, retinal blindness, glaucoma, ocular repair, ophthalmic pathology, retinal development, inflammatory eye disease and more.
The institute is well placed, through its combined clinical and research-based strategies, to apply expertise from across the University in genome engineering, sequencing, vector and stem cell technology, to these issues causing blindness.
“For diseases of the eye’s window – the cornea – we are also finding solutions,” Professor McCluskey says. “This is critical, as corneal disease is a leading cause of irreversible visual impairment that affects all ages.”
Professor Stephanie Watson’s team at the institute has developed therapies to treat corneal disease. Stem cell therapies have restored sight and, for corneal infection (keratitis), new models of care are reducing the burden on both the patient and the health system.
“We have also created ‘Save Sight Registries’ to track the progress and outcomes for people being treated for these diseases in real time,” says Professor McCluskey. “The module for macular degeneration is the largest, prospectively gathered database of patient outcomes for treatment of macular degeneration in the world.”
The data being gathered from the registries is leading to a better understanding of outcomes, and is changing the way these diseases are treated. Much of Save Sight Institute’s research is conducted thanks to the generosity of people like Ms Diana Mackintosh.
How you can help
If you would like more information on how to support the Save Sight Institute, please contact the Planned Giving team on +61 2 8627 8824, or online at savesightinstitute.org.au
