Gut feeling
New research into the human gut and its trillions of inhabitants could undo some of the confusion around healthy eating and address a surprising range of the modern world's most difficult medical conditions.
Inside you right now an estimated 39 trillion microbes comprising 1000 species are breaking down food and toxins, manufacturing vitamins and influencing your immune system. And this microbe empire is vast. The surface area of your gut is up to 100 times greater than the surface area of your skin.
“The gut is the largest immune organ, the largest endocrine organ, and the second largest neural organ – second only to the brain,” says Associate Professor Andrew Holmes, who specialises in microbial ecology. “It’s where you have this – more or less – seamless connection from diet to microbes to metabolic health to immune health.”
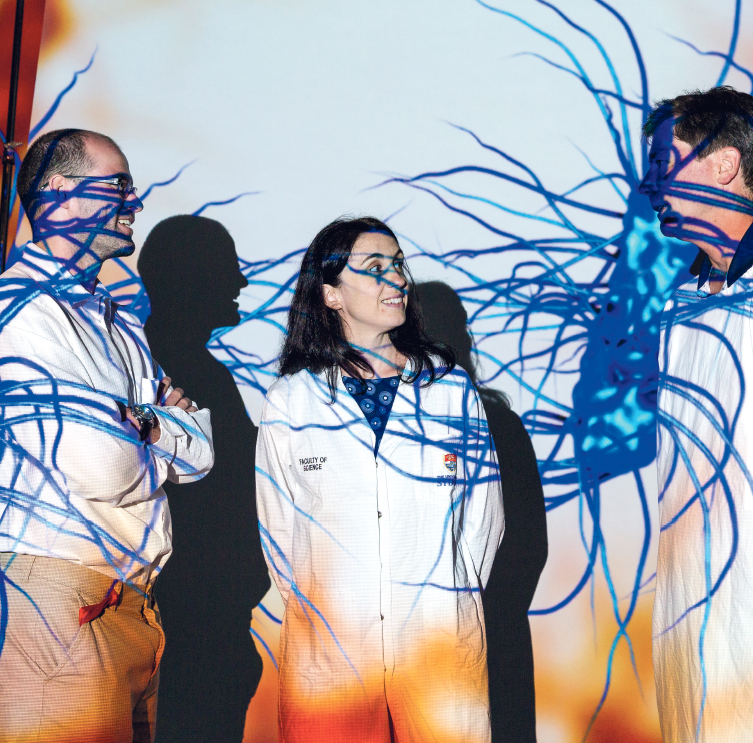
Projections of microbes from the microbiome. The cross-disciplinary team working to understand the human gut.
People are becoming more aware of the health implications of what happens in the gut. But still these microbes are seen as part of a gurgling swamp of unspeakable substances. When things go wrong, you clean it up by adding some good guys or removing some bad guys.
Professor Holmes sees it very differently. “It’s more like a rainforest restoration,” he says. “You don’t restore a complex system by adding or subtracting a few species.”
These ideas are part of a new frontier in medical research that promises different and better options for how we treat everything from obesity to arthritis and emotional disorders.
In the womb, we are microbe free. When we enter the world, it takes about five years to acquire our own distinctive set of microbes. What we eat, the stage of our immune development and the microbes we are exposed to through family and friends and many other sources, are all key influences on the process.

Dr Mark Read
In research circles, the gut ecosystem is termed the microbiome and its trillions of inhabitants are the microbiota. The human alliance with microbes goes back a long time. They’ve lived within us since our very, very distant ancestors evolved beyond being microbes themselves. In fact, evolution factored in the action of microbes when it designed our bodies: for example, 10 percent of our energy is supplied through the work of microbes.
Microbes are choosy about where they live. We have roughly 2 kilograms of microbes in our bodies, nearly the weight of the brain, but most of them prefer to live in the large intestine, also called the colon. After the small intestine has absorbed most of the sugar, fat and protein that’s easily available in what we eat, what’s left – a range of materials given the general name ‘fibre’ – is met by hordes of bacteria in the colon. As they tear apart otherwise indigestible molecules they generate what are called short-chain fatty acids, which our bodies need for almost everything to do with metabolism, behaviour and immune function.
Now you can't put a peanut in a school lunchbox because of food allergies. In the past 20 years, something went wrong.
So what happens if a reduced amount of fibre makes it through the small intestine to feed the microbes in the colon? This isn’t a theoretical question. It is essentially thecontinuing experiment of the Western diet. People eating traditional diets receive 60 to 120 grams of fibre a day to support a diverse community of microbes. Even a ‘healthy’ Western diet may supply only 10 to 15 grams. Our processed foods are so easily digestible in the small intestine that gut bacteria further along starve, disrupting the metabolic and immune systems.

Dr Laurence Macia
Dr Laurence Macia is an immunologist and she leads a team at the Charles Perkins Centre that closely collaborates with Professor Holmes. At the centre researchers across a number of disciplines focus on the modern lifestyle diseases that are already threatening to overwhelm healthcare budgets and send life expectancy backwards.
“There was a time when we were less sick,” Dr Macia says with a look of alarm. “Now you can’t put a peanut in a school lunchbox because of food allergies. In the last 20 years, something went wrong.”
Part of her research involves varying the diets given to mice then looking for changes in their droppings, microbiome, immune cells and health profiles. “We have already published our findings,” Dr Macia says in her warm French accent. “It is clear that mice on low-fibre diets develop a massive peanut allergy compared to mice fed on high-fibre diets.”
Dr Macia believes that understanding how our gut microbes communicate with our immune cells will be critical to developing new treatments or preventing most non-communicable Western diseases.

Associate Professor Andrew Holmes
Advances in DNA sequencing about 10 years ago really opened up the microbiome as a practica eld of study. Helping take it forward now are technologies around artificial intelligence and big data that can make sense of the staggering number of touch points in the functioning of the microbiome. This is where Dr Mark Read comes into the picture. True to the Charles Perkins Centre’s multidisciplinary culture, Dr Read is a computer scientist who sounds a little surprised, though excited, to be where he is.
“When I was studying I heard about people building computational algorithms and solutions inspired by biology, which I found fascinating and slightly crazy,” he says. “Now I’m applying some of these techniques to solve biological problems.”
He explains the challenges of getting a handle on the microbiota. “There are many different species of bacteria in your gut. So you’re trying to spot patterns across diets captured in spreadsheets with thousands of columns. Now, what if you want to vary that around say, different kinds of fat in the diet? Data grows exponentially with each additional variable.”
Computers also allow the running of simulations. So instead of weeks of manipulating diets and collecting droppings, the consequences of diet variations can be established almost instantly.

Associate Professor Andrew Holmes, Dr Laurence Macia and Dr Mark Read
For all the progress and incredible possibilities, Professor Holmes is quick to point out that harnessing the microbiome is not a silver bullet for health because we are also affected by other modern factors such as stress, lack of exercise and sleep deprivation.
“It’s the interaction of everything that determines how the whole system is going to work,” he says.
It’s still early days. That’s where Professor Holmes, Dr Macia and Dr Read are right now: on the edge of a rainforest, taking the first few, eager steps in.
How to get involved
This new research has implication for everything from diabetes to depression. If you would like to learn more or support our researchers, please contact Lachlan Cahill, ph (02) 8627 8818 or email development.fund@sydney.edu.au
Written by George Dodd
Photography by Louise Cooper
