The 3D printing revolution in orthopaedic devices for children
Most orthopaedic devices only come in adult sizes, but using biomedical engineering, Dr Tegan Cheng is changing that. Based at Westmead and using 3D printing, her most useful tools are imagination and determination.
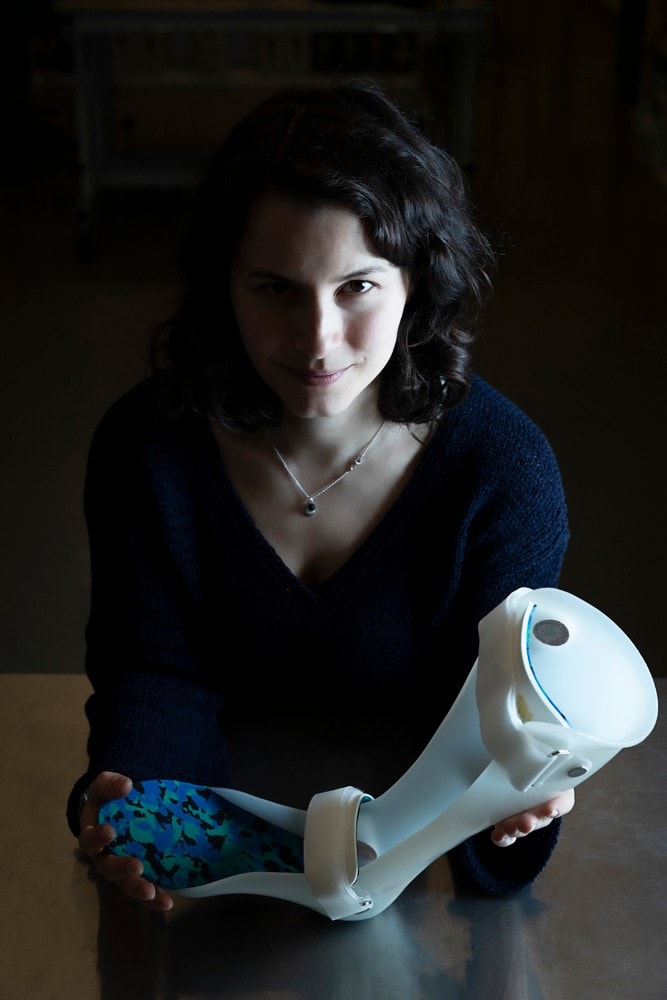
Holding a current-style plaster and thermoplastic orthotic, Cheng is working on how to 3D print these devices for much greater precision and speed of production.
When parents are told their child has a neuromuscular disease like spastic cerebral palsy, it’s a challenging enough fact to deal with without then learning that the treatment options for their child are limited. Happily, solutions are emerging, but first, some background on the condition itself.
For children with cerebral palsy, messages going to the muscles get scrambled as they travel through damaged neurons in the brain and spinal cord. Over time, this scrambling changes the associated muscles, tendons and ligaments, causing stiffening or atrophy. When a child’s wrists are affected, it can pull their hand inwards like a hook, making it hard for them to wash or get dressed without pain or discomfort.
An often-used option is to have a wrist plate implanted to straighten the wrist and improve quality of life, but these implants are only made in adult sizes. Surgeons helping children have to do the best they can with devices that aren’t really fit for purpose.
That’s where Dr Tegan Cheng comes in. Immediately likeable, with a bright, let-me-help energy, Cheng’s specialities are problem solving and curiosity. That curiosity led her to explore undergraduate degrees in biomedical engineering and medical science, as well as a PhD in bone tissue engineering – basically growing bone out of nothing. As the University’s first dual lecturer in both engineering and medicine, Cheng is no academic lightweight and she brings all her skills to bear in helping children across some difficult treatment hurdles.

How a 3D printer sees Tegan as it is being readied to 3D print her image.
“Surgeons were getting very frustrated at having to use adult plates on these kids, sometimes bending or manipulating them in surgery. You know the plates are going to be too big and are going to irritate the kid, but there's no alternative,” says Cheng, who’s the manager of the Engineering and Prototyping of Implants for Children Laboratory, also known as the EPIC Lab, at the Children’s Hospital at Westmead.
The EPIC Lab was set up in 2016 by orthopaedic surgeon, Professor David Little, to develop off-the-shelf specialty orthopaedic or musculoskeletal implants for children. Situated on the same floor as the Children’s Hospital at Westmead, and in the building next door to the Westmead adult hospital, the lab is well placed to puzzle out the full range of challenging orthopaedic issues.
For Cheng putting these puzzles together demands input from a range of specialists.
“With our implants, we've taken on a user-focused approach, so we talk to different surgeons at different levels, as well as orthotists, physios, mechanical engineers and computer scientists,” she says.
Working in a lab dotted with 3D printed replicas of everyone on the team, as well as team mascot, Jack Skellington (yes, he’s a skeleton), Cheng and the team came up with the Wrist Fusion Plate System.
The device was one of the first the lab developed in collaboration with US company OrthoPediatrics as part of its range of orthopaedic devices for children. The plates are low-profile under the skin, which helps reduce irritation of soft tissue. The system also comes in two lengths to allow for patients who’ve had a procedure called proximal row carpectomy (PRC) for degeneration of the wrist.
“There isn’t a huge financial incentive to develop new devices specifically for children’s orthopaedic devices as the market is really small. However, it’s an important niche,” says Cheng. “We had this boring project to make a really small version of the adult device. But the impact it will have on children is huge.”

Wrist plates can work wonders for children with neuromuscular diseases, but they only come in adult sizes.
When Cheng says “boring”, that just means “easier than some of my other projects”. These have included designing devices that help to correct the way bones grow, or brainstorming ways of redesigning a device that has a tendency to fail. It’s tricky stuff made trickier by the fact that children tend to be more active than adults with more bumps and falls, and bones that are smaller and still growing.
Getting an implant right the first time can mean less surgery down the track. “We want to make the operations these kids have less invasive and less traumatic by creating minimally invasive devices that work in a low impact way,” Cheng says.
To do this, Cheng came up with a research program to improve children's orthopaedic care through 3D printing and design. For children with particular walking difficulties, it incorporates machine learning, where the results of every treatment are used to educate an algorithm that will predict the most suitable avenues to pursue in future cases.
The ideas for the devices are often driven by Professor Little who returns from surgery talking about the children he is treating, and how the implants available just aren’t suitable.

3D printed Teng, with others from the research team in the background.
The team will think about a possible solution, draw it up in the computer, and 3D print it to test it, usually by mechanical testing within the lab using foam bones.
Having the lab so close to the Children’s Hospital means that Cheng can run down the hall to the operating theatre, catch Little between operations, show him the design and then run back again, tweaking and reprinting it until it is right. In the few short years that the lab has been open, it has developed an impressive swag of new devices now in the process of being commercialised. For children who would otherwise face years of operations, the devices can’t come soon enough. For Cheng, it’s the job of her dreams.
“I would never have guessed that this is where I would have ended up. It’s a far cry from bone tissue engineering,” she says. “The goal of every day of our lives is to try and make these kids’ lives a little bit better.”