
Culturally diverse people might resist frontotemporal dementia symptoms for longer
Findings suggest language and an active lifestyle play a role in buffering against dementia
University of Sydney researchers who compared people with frontotemporal dementia have found that those born overseas who first spoke a language other than English can tolerate the disease longer before symptoms gain a foothold.
The researchers have called for more sophisticated diagnostic criteria and clinical record keeping to address their findings.
The study led by Ms Amira Skeggs, a clinical researcher in the School of Psychology, has been published in the Journal of Neurology. It focuses on one of three types of the disease known as behavioural variant frontotemporal dementia (bvFTD). In February, American actor Bruce Willis announced he had been diagnosed with frontotemporal dementia.
“Frontotemporal dementia refers to a set of younger-onset dementia syndromes, which are typically diagnosed before the age of 65,” Ms Skeggs said.
“Our findings suggest that current diagnostic methods might be less accurate at identifying symptoms in Australians from culturally diverse backgrounds.
“When it comes to neurodegenerative syndromes like bvFTD, culturally diverse people can have a later onset of the disease compared to monolingual Australians because they have other factors which could increase their resilience or cognitive reserve.”
Cognitive reserve is a kind of fortification that helps the brain weather progression of neurodegeneration before symptoms of mental decline emerge. This reserve is built up over an active lifetime and is influenced by a range of factors.
“There is a tendency for culturally diverse patients, particularly those who come to Australia, to have higher levels of cognitive reserve,” Ms Skeggs said.
“Multilingualism, education, working in a complex profession for a long time, all of these factors add up and make you more resilient to cognitive decline – up to a point.
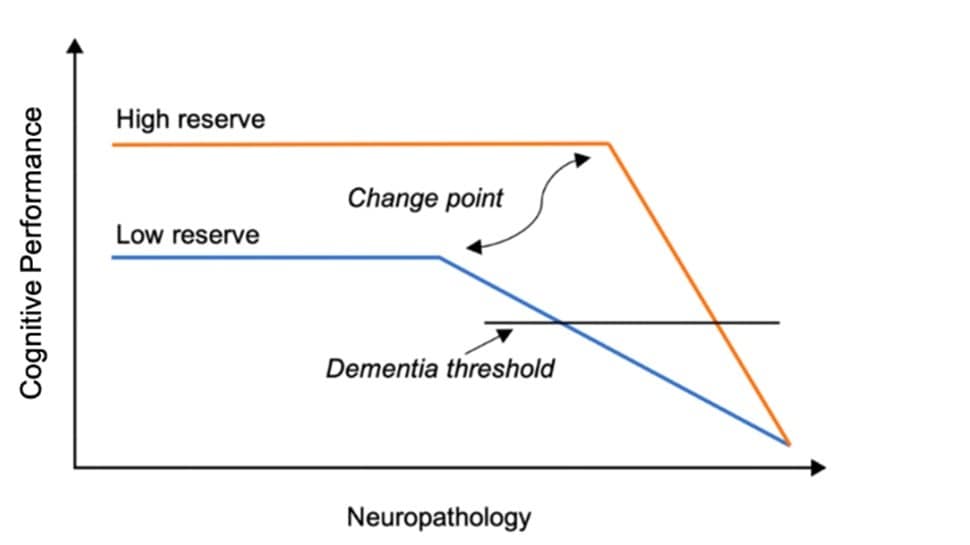
Hypothesised change in cognitive function over time in individuals with high and low cognitive reserve, adapted from Bialystok, 2021
“The downside of this cognitive reserve is that it may cause diagnosis to be delayed or mistaken. At the point where the disease becomes visible to others, the patient’s cognition may decline steeply because they have had a sustained period of brain atrophy without it being addressed.”
BvFTD is a progressive neurodegenerative disease that affects brain areas responsible for behaviour, personality, language and emotions. Degeneration of nerve cells in the brain leads to the loss of function in these areas, typically starting gradually and worsening over time.
In the study, researchers compared clinical symptoms of people with bvFTD based on culture and language for the first time. The 107 participants were separated into three groups: Australians who speak only English and two groups of culturally diverse people, one that spoke English as their first language and another that spoke a different tongue in the beginning.
“Comparisons revealed that the group who spoke a non-English first language performed worse than the other groups on verbal tests but better on non-verbal tests,” Ms Skeggs said.
“The poor verbal performance in the non-English speaking group is probably influenced by cultural biases within current clinical tests, so the reason they are showing decline may not actually be because they are declining.”
![Verbal and non-verbal cognitive scores for Australian, CALD-English (culturally diverse people who spoke English as their first language) and CALD-LOTE (culturally diverse people who spoke non-English as their first language) groups [Credit: Skeggs et al.]](/content/dam/people/students/non-professional/figure-3_revised.jpg/_jcr_content/renditions/cq5dam.web.1280.1280.jpeg)
Verbal and non-verbal cognitive scores for Australian, CALD-English (culturally diverse people who spoke English as their first language) and CALD-LOTE (culturally diverse people who spoke non-English as their first language) groups [Credit: Skeggs et al.]
Ms Skeggs said an interesting finding emerged where bilingual patients lost their second language.
“We had one Vietnamese patient who spoke English perfectly before disease onset, but by the time the disease had progressed, he had completely lost his English ability and could only communicate in Vietnamese, even though he had been speaking English perfectly for over 50 years,” she said.
A major healthcare shortfall that needs to be updated for people with bvFTD, Ms Skeggs said, is the skewed diagnostic criteria, which has almost been built entirely on Western profiles. In Australia 29 percent of the population is born overseas.
“At the moment we probably don’t have an accurate and valid way of diagnosing symptoms or disease in culturally and linguistically diverse people,” Ms Skeggs said.
“Currently, all the diagnostic criteria are based off Western samples, which means that it can be difficult to diagnose the diseases in non-Western people because they may not have the same symptoms.
“There is also some evidence that non-English-speaking patients are diagnosed at a later age, potentially due to a delay in clinical diagnosis or cognitive reserve slowing the disease onset.”
The researchers said clinics should be collecting information about a patient’s cultural background, bilingualism and education, and offer alternatives during diagnosis such as a translator or image-based testing.
The study was conducted at FRONTIER Research Group, Australia’s largest specialist clinic for frontotemporal dementia.
DOI: https://doi.org/10.1007/s00415-023-11638-w
Declaration: This study was supported by ForeFront, a large collaborative research group dedicated to the study of neurodegenerative diseases and funded by the National Health and Medical Research Council of Australia Program Grant, Dementia Research Team Grant, and the ARC Centre of Excellence in Cognition and its Disorders.