How the CPAP machine beats deadly sleep apnoea

Professor Colin Sullivan in the foyer of the Blackburn Building, one of the first places in the world where clinicians were also researchers.
It’s now considered one of the most significant medical advances of the 20th century, but at the time of its creation, no-one could have imagined the impact the continuous positive airway pressure (CPAP) machine would have. Not even its inventor, Professor Colin Sullivan (BSc (Med) ’67 MBBS ’70 PhD (Med) ’77).
“Most people were thinking in terms of a surgical solution to sleep apnoea,” Sullivan says, sitting in the very rooms of the University of Sydney’s Blackburn Building where he investigated the condition and painstakingly built the first CPAP device. “The machine was an experiment, but the experiment turned into the treatment.”
In some areas of research, if you fail, you might just move on to something else. But if you’re also a clinician, you still have a patient there. You have to keep working to solve the problem.

Polygraph machines are best known for spotting untruths. In the early days, Sullivan used this machine to measure blood pressure, pulse and respiration in sleeping patients.
As Sullivan speaks, you can clearly sense his dedication, his compassion for his patients and how energised he is by his work. Ironically, in the early days, he didn’t get much sleep either. He worked long hours, conducting sleep studies on his patients well into the night, followed by clinical work the next morning. Even now, there are too few hours in the day as he shares his time between not just research and clinical work, but also teaching. In fact, during his career, Sullivan has guided and encouraged more than 46 PhD students.
Work on CPAP started in the late 1970s when Sullivan was a University of Sydney researcher and a clinician at Royal Prince Alfred Hospital, mostly looking after people with respiratory failure, often caused by unrecognised sleep apnoea. Internationally, a handful of people were studying sleep, but no-one thought to look at how breathing behaves during sleeping hours. The doorway in for Sullivan was a colleague’s contact with Sudden Infant Death Syndrome (SIDS).
“The notion with these babies was that something happened to their breathing when they were asleep,” Sullivan says. “So we started researching the physiology of their breathing. At the time we had no idea that thousands of adults had breathing problems during sleep as well.”
In fact, when Sullivan made the connection with adults, sleep apnoea was considered so rare that hospital authorities wouldn’t provide much in the way of resources to study it. Sullivan had to borrow, improvise and invent the equipment he needed.
Of course, sleep apnoea was never rare. It was hiding in sleepy spouses and snoring grandparents. Family and friends would often make light of symptoms we now know are signs the body is under tremendous strain, enough to be debilitating or even deadly.
“Most people were thinking in terms of a surgical solution to sleep apnoea. The machine was an experiment, but the experiment turned into the treatment.”

At a time when few people knew they had sleep apnoea, Sullivan sometimes had to use himself as a test subject.
One of Sullivan’s early patients was in the life-threatening stage of the condition, yet he refused the only treatment at the time: a tracheostomy, where a hole is made through the neck into the trachea so breathing can bypass the nose and mouth. “I said, ‘Look, you really have to have this, or the apnoea will kill you’,” Sullivan recalls, still with a sense of alarm.
For this patient, the cure was worse than the disease, especially since the only symptom he thought he had was sleepiness. His blood chemistry told a different story. The blood oxygen levels of a sleeping person in the grip of apnoea can drop by 50 percent. That’s like being at the top of Everest, which would normally cause an awake person to pass out or even die.
Since the patient refused the operation, Sullivan decided to try an idea he’d had where the patient’s airways would be gently pressurised, like a splint keeping airways open.

The workshop where Sullivan worked with Jim Bruderer. Sullivan himself had to be electrician, designer, metallurgist, even upholsterer, wielding the needle to fix the fabric of the bed used for sleep studies.
Sullivan came from a mechanically minded family. His mother was a milliner, his father was an electrician who worked on ships at Sydney’s Cockatoo Island and his two older brothers became successful engineers. So it wasn’t surprising that his idea for tackling apnoea was non-surgical.
“I asked my patient, ‘Are you happy to do an experiment? I want to test this idea and it might help you.’ He agreed to do it, and it worked,” Sullivan says.
Sullivan found he was able to turn his patient’s apnoea on and off with the machine, an effect which today makes it invaluable for researchers in the field of sleep disordered breathing (SDB); a field initiated by Sullivan’s work. For that first patient, the results were dramatic. His oxygen levels normalised, his respiration and cardiac function improved, and for the first time in many years, he was getting enough sleep. This, of itself, changed his life.
That first success kick-started an energetic process of research and invention. Helping Sullivan were his first two PhD students, Faiq Issa (PhD(Med) ’85) and Mike Berthon-Jones (MBBS ’77 PhD(Med) ’87), who set about measuring the significant improvements resulting from CPAP treatment. Later came people now considered world authorities on sleep: Dr Ron Grunstein (MBBS ’80 MD ’95), Dr Peter Cistulli (PhD(Med) ’95), who published original research on oral appliances and is the University’s first Professor of Sleep Medicine, and Professor Karen Waters (PhD(Med) ’94), who researches sleep apnoea in children and also SIDS.

Sleep studies involved measuring the patients’ vital signs. This equipment was used to amplify the signs to reveal more information.
Another key member of the team was a retired Swiss-trained toolmaker, Jim Bruderer. He and Sullivan worked together in a CPAP machine workshop in the Blackburn Building, constantly producing improved CPAP masks as they were needed.
“People were always asking, ‘Why don’t you outsource that?’ But doing everything right here, responding almost instantly to what we found we needed – you just can’t have that immediacy if you’re outsourcing,” Sullivan says.
All this led to the opening of the world’s first sleep apnoea clinic at Royal Prince Alfred Hospital, allowing patients to take their CPAP machines home. By 1985, a hundred people were on the program, but interest stayed mostly local. Further afield, clinicians were interested in the concept for research purposes, but doubted if patients would use what was then a loud and cumbersome machine, long term.
It was also still widely thought that surgery would ultimately provide the answer.
That surgical answer is yet to come but by 1989, one thousand patients were using machines built in the Blackburn Building workshop. Both Sullivan and the University’s Business Liaison Office could see the potential of the device, and indeed for an Australian medical device company. On this basis, an offer in 1985 was refused from the CEO of Respironics (now Phillips), the first company in the United States to market a system based on Sullivan’s original 1981 publication in the leading British medical journal, The Lancet.
Not long after, Sullivan began working with Dr Peter Farrell (BE(Chem) ’64), who was looking for investment opportunities in medical advances. This led to the first commercial production of the machine through a company called ResCare, which later became ResMed. A major advance emerged in 1990 from the ongoing work by Sullivan and Bruderer in the form of a new design element called the “bubble mask”. This provided a new level of comfort and sealing, and gave a competitive advantage as the nascent ResCare entered the major US market.
Starting with just nine employees in 1989, ResMed now employs well over 6000 people, operates in 100 countries and is considered one of the most successful commercialisations of a medical advance ever achieved.
Sullivan has had a long association with the University of Sydney, which began with him being taken to an open day when he was a teenager. For the first time, he became aware of the science of physiology, which deals with the mechanics of the human body. Sullivan had found his path. He excelled at his studies and went on to demonstrate drive, initiative and creative thinking in everything he did.
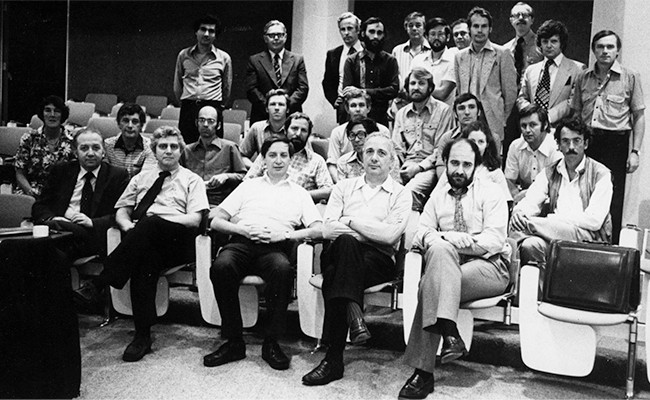
Taken in the early 1980s, this photo shows a meeting of almost all the sleep researchers in the world at the time. Today, there are more sleep researchers at the University of Sydney, alone.
Another vital ingredient of his work, and something he believes in passionately, is the University of Sydney’s bridge between medical research and clinical treatment. When the Blackburn Building opened in the 1930s thanks to a grant from the Rockefeller Foundation in the United States, that bridge was literal, with a footbridge allowing researchers to walk from what was then the Rockefeller New Medical School Building, to Royal Prince Alfred Hospital.
At the time, it was a radical idea for researchers to have clinical patients. Today it’s best practice and for good reason. “In some areas of research, if you fail, you might just move on to something else,” Sullivan says. “But if you’re also a clinician, you still have a patient there. You have to keep working to solve the problem.”
Indeed throughout his career, Sullivan has been a gifted problem solver for himself and others. As previously mentioned, his work opened up the field of sleep disordered breathing, with implications for conditions such as dementia, the surprisingly common childhood apnoea, and the many causes of respiratory failure. Perhaps most dramatically, a person with polio or muscular dystrophy no longer has to stay locked in an iron lung. The modern, super-compact CPAP machine, gives them a freedom that was previously impossible.
Sullivan’s current research is on obstructed breathing during pregnancy, which pushes up maternal blood pressure, reduces the amount of oxygen reaching the foetus and can compromise foetal growth.
So, well beyond the benefits of treating sleep apnoea, the significance of Sullivan’s work has been profound.
“I received a letter from someone in the United States yesterday, saying thank you. I feel quite ...” he hesitates, struggling to find the right word as he’s caught between the huge impact of his invention and his natural humility. “I mean, it’s wonderful to be part of this. I feel this is wonderful.”
