
Hyper-intense white matter in brain found in frontotemporal dementia
A University of Sydney study has found the amount of white matter hyperintensities in the brain is associated with severity of frontotemporal dementia.
Areas of brain damage called white matter hyperintensities are commonly linked to vascular/blood vessel-related health problems and have also been linked to Alzheimer’s disease. Now a study has shown that white matter hyperintensities are also found in frontotemporal dementia. Frontotemporal dementia, which often affects people under the age of 65, mainly results in changes in personality, behavior and problems with language rather than memory.
The University of Sydney study publishes today in Neurology®, the medical journal of the American Academy of Neurology.
The senior author, Dr Ramón Landin-Romero, from the Brain and Mind Centre said: “We were expecting to see similar amounts of white matter hyperintensities in frontotemporal dementia and Alzheimer’s disease, but we actually found higher levels in people with frontotemporal dementia.
“We also expected to see that people with more severe disease would have more white matter hyperintensities, regardless of disease, but that was only true in people with frontotemporal dementia,” said Dr Landin-Romero, from the School of Psychology in the Faculty of Science.
The amount of white matter hyperintensities was associated with the severity of a person’s frontotemporal dementia, including the severity of their symptoms and everyday difficulties, but it was not associated with having vascular risk factors such as high blood pressure and high cholesterol as was expected.
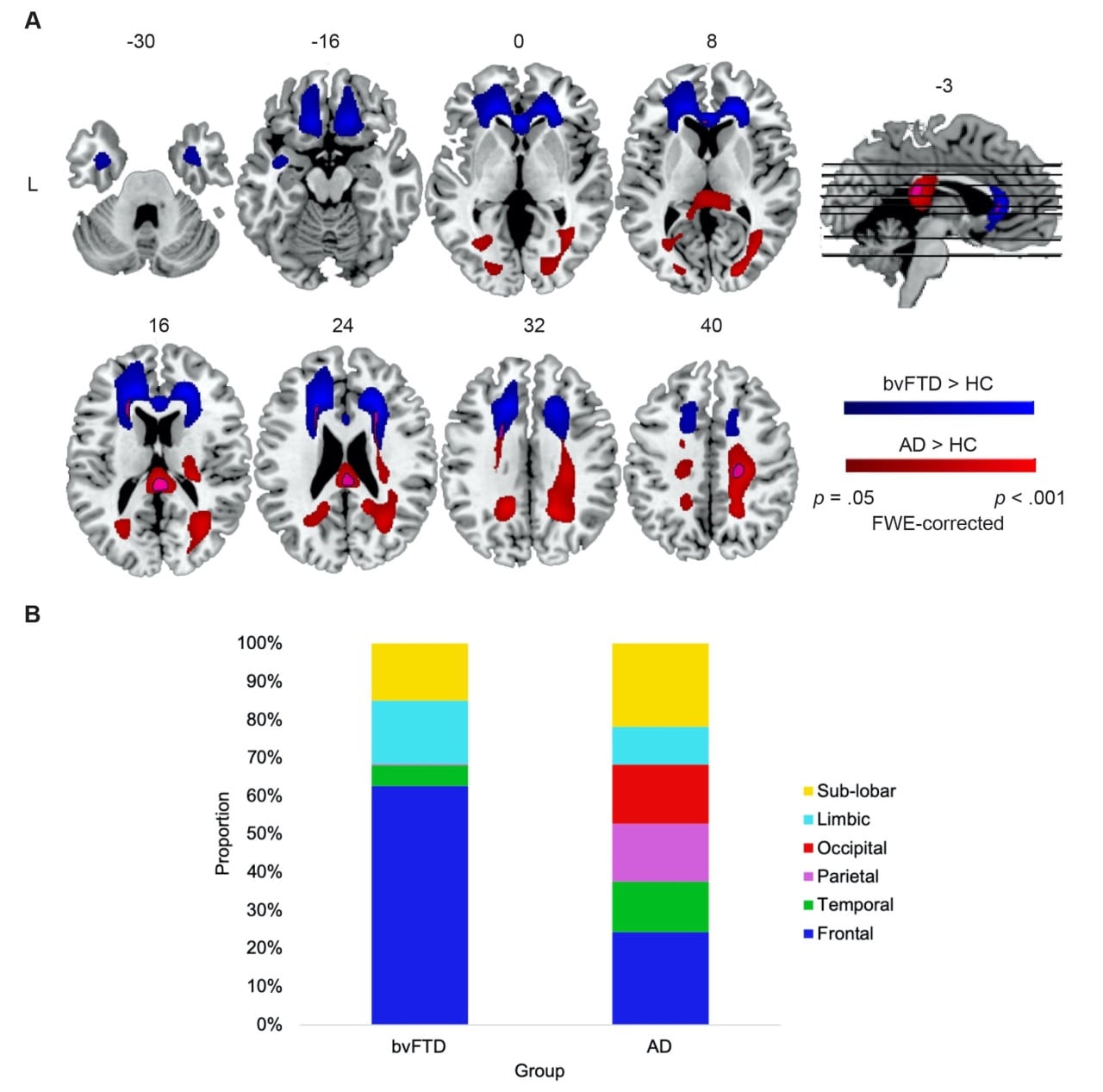
The coloured areas represent the white matter hyperintensities in frontotemporal dementia (blue) and Alzheimer’s disease (red).
“In general, white matter hyperintensities have been associated with these vascular risk factors, so these results suggest that white matter hyperintensities are partly independent of vascular factors and associated with the progressive loss of brain integrity, more specifically the loss of brain cells, due to frontotemporal dementia,” Dr Landin-Romero said.
The researchers also found that higher amounts of white matter hyperintensities in certain areas of the brain were associated with worse cognitive performance.
For example, in both frontotemporal dementia and Alzheimer’s disease, increased white matter hyperintensities in the corpus callosum, a bundle of white matter fibers connecting the left and right hemispheres of the brain, was associated with attention problems.
“White matter hyperintensities should be viewed as a core feature of frontotemporal dementia and Alzheimer’s disease that can contribute to cognitive problems, not simply a marker of vascular disease,” Dr Romero-Landin concluded.
About the study
The study involved 64 people with frontotemporal dementia, 65 people with Alzheimer’s disease and 66 people without dementia who had brain scans and other tests. Participants were followed for an average of two years. Autopsy information was available for 13 of the people with frontotemporal dementia and five of the people with Alzheimer’s disease.
The researchers found that the total volume of white matter hyperintensities in the brain was larger in people with frontotemporal dementia than in the people with Alzheimer’s disease or the healthy control group. The average volume of white matter hyperintensities in people with frontotemporal dementia was 0.76 milliliters (mL) compared to 0.40 mL in people with Alzheimer’s disease and 0.12 mL in people without dementia.
A limitation of the study was that autopsy information was available for only a small number of cases, so the underlying molecular cause of the white matter hyperintensities could not be determined for participants.
Disclaimer
The study was supported by the National Health and Medical Research Council of Australia and by the Appenzeller Neuroscience Fellowship in Alzheimer’s disease.
